
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
Response
- Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography (Diabetes Metab J 2023;47:104-17)
- Hwi Seung Kim, Hong-Kyu Kim, Chang Hee Jung
- Diabetes Metab J. 2023;47(2):304-305. Published online March 15, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0058
- 1,647 View
- 119 Download
- 1 Crossref
Original Article
- Metabolic Risk/Epidemiology
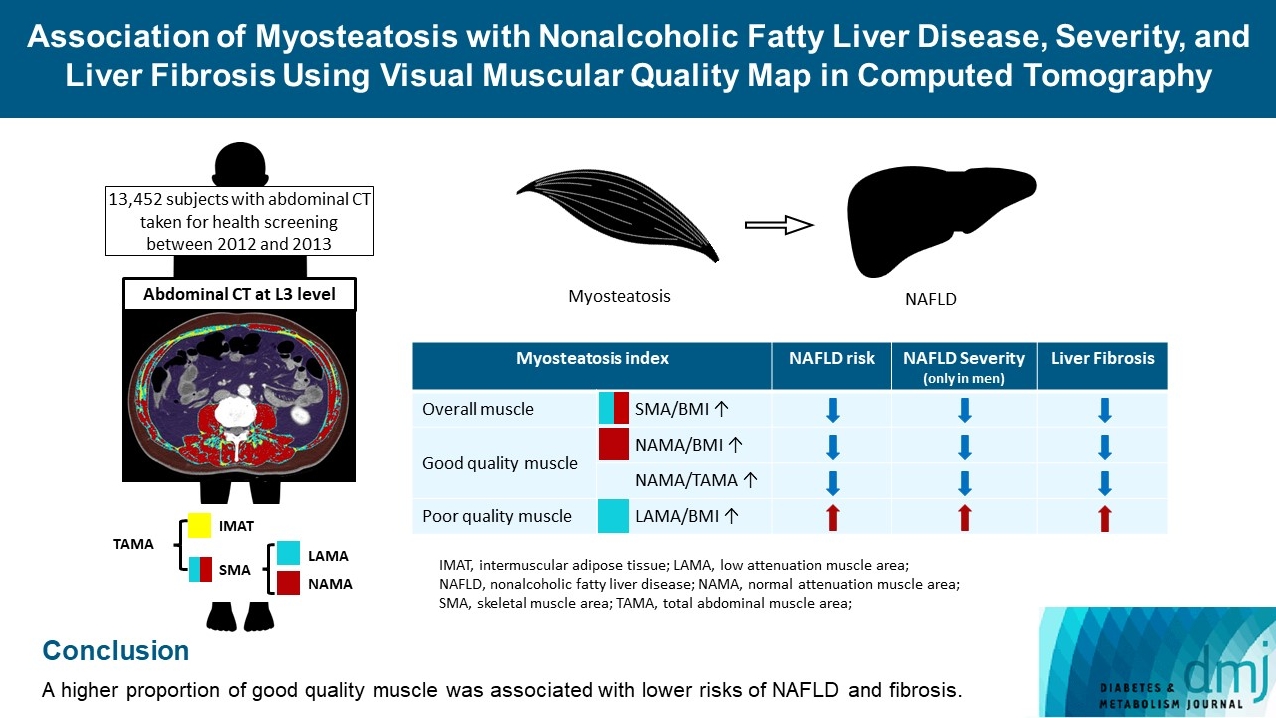
- Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography
- Hwi Seung Kim, Jiwoo Lee, Eun Hee Kim, Min Jung Lee, In Young Bae, Woo Je Lee, Joong-Yeol Park, Hong-Kyu Kim, Chang Hee Jung
- Diabetes Metab J. 2023;47(1):104-117. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0081
- 3,276 View
- 176 Download
- 7 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The association of myosteatosis measured using visual muscular quality map in computed tomography (CT) with nonalcoholic fatty liver disease (NAFLD), its severity, and fibrosis was analyzed in a large population.
Methods
Subjects (n=13,452) with abdominal CT between 2012 and 2013 were measured total abdominal muscle area (TAMA) at L3 level. TAMA was segmented into intramuscular adipose tissue and skeletal muscle area (SMA), which was further classified into normal attenuation muscle area (NAMA) and low attenuation muscle area (LAMA). The following variables were adopted as indicators of myosteatosis: SMA/body mass index (BMI), NAMA/BMI, NAMA/TAMA, and LAMA/BMI. NAFLD and its severity were assessed by ultrasonography, and liver fibrosis was measured by calculating the NAFLD fibrosis score (NFS) and fibrosis-4 index (FIB-4) scores.
Results
According to multiple logistic regression analyses, as quartiles of SMA/BMI, NAMA/BMI, and NAMA/TAMA increased, the odds ratios (ORs) for NAFLD decreased in each sex (P for trend <0.001 for all). The ORs of moderate/severe NAFLD were significantly higher in the Q1 group than in the Q4 group for SMA/BMI, NAMA/BMI, and NAMA/TAMA in men. The ORs of intermediate/high liver fibrosis scores assessed by NFS and FIB-4 scores increased linearly with decreasing quartiles for SMA/BMI, NAMA/BMI, and NAMA/TAMA in each sex (P for trend <0.001 for all). Conversely, the risk for NAFLD and fibrosis were positively associated with LAMA/BMI quartiles in each sex (P for trend <0.001 for all).
Conclusion
A higher proportion of good quality muscle was associated with lower risks of NAFLD and fibrosis. -
Citations
Citations to this article as recorded by- Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography (Diabetes Metab J 2023;47:104-17)
Hwi Seung Kim, Hong-Kyu Kim, Chang Hee Jung
Diabetes & Metabolism Journal.2023; 47(2): 304. CrossRef - Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography (Diabetes Metab J 2023;47:104-17)
Eun Roh
Diabetes & Metabolism Journal.2023; 47(2): 301. CrossRef - Sarcopenia, a condition shared by various diseases: can we alleviate or delay the progression?
Giovanni Tarantino, Gaia Sinatti, Vincenzo Citro, Silvano Santini, Clara Balsano
Internal and Emergency Medicine.2023; 18(7): 1887. CrossRef - Association of Visceral Fat Obesity, Sarcopenia, and Myosteatosis with Non-Alcoholic Fatty Liver Disease without Obesity
Hong-Kyu Kim, Sung-Jin Bae, Min Jung Lee, Eun Hee Kim, Hana Park, Hwi Seung Kim, Yun Kyung Cho, Chang Hee Jung, Woo Je Lee, Jaewon Choe
Clinical and Molecular Hepatology.2023; 29(4): 987. CrossRef - Current view of the surgical anatomy of the anterolateral abdominal wall muscles and their aponeuroses
A.V. Pavlov, A.S. Baranova, A.V. Fedoseyev, A.I. Vvedensky, G.S. Lazutina, N.V. Ovchinnikova, I.V. Bakharev
Operativnaya khirurgiya i klinicheskaya anatomiya (Pirogovskii nauchnyi zhurnal).2023; 7(3): 44. CrossRef - Muscle Fat Content Is Associated with Nonalcoholic Fatty Liver Disease and Liver Fibrosis in Chinese Adults
W. Guo, X. Zhao, D. Cheng, X. Liang, M. Miao, X. Li, J. Lu, N. Xu, Shuang Hu, Qun Zhang
The Journal of nutrition, health and aging.2023; 27(11): 960. CrossRef
- Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography (Diabetes Metab J 2023;47:104-17)
Response
- Clinical Efficacy of Sodium-Glucose Cotransporter 2 Inhibitor and Glucagon-Like Peptide-1 Receptor Agonist Combination Therapy in Type 2 Diabetes Mellitus: Real-World Study (Diabetes Metab J 2022;46: 658-62)
- Hwi Seung Kim, Woo Je Lee
- Diabetes Metab J. 2022;46(4):665-666. Published online July 27, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0166
- [Original]
- 2,435 View
- 130 Download
- 1 Web of Science
- 1 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Type 2 diabetes mellitus pharmacological remission with dapagliflozin plus oral semaglutide
Maria Elena Lunati, Vincenzo Cimino, Davide Bernasconi, Alessandra Gandolfi, Paola Silvia Morpurgo, Camilla Tinari, Elisa Lazzaroni, Laura Baruffaldi, Milena Muratori, Laura Montefusco, Ida Pastore, Antonio Rossi, Ivano Giuseppe Franzetti, Fabrizio Murato
Pharmacological Research.2024; 199: 107040. CrossRef
- Type 2 diabetes mellitus pharmacological remission with dapagliflozin plus oral semaglutide
Short Communications
- Drug/Regimen
- Clinical Efficacy of Sodium-Glucose Cotransporter 2 Inhibitor and Glucagon-Like Peptide-1 Receptor Agonist Combination Therapy in Type 2 Diabetes Mellitus: Real-World Study
- Hwi Seung Kim, Taekwan Yoon, Chang Hee Jung, Joong-Yeol Park, Woo Je Lee
- Diabetes Metab J. 2022;46(4):658-662. Published online November 8, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0232
- 65,535 View
- 387 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Sodium-glucose cotransporter 2 inhibitor (SGLT2i) and glucagon-like peptide-1 receptor agonist (GLP-1RA) are novel anti-diabetic drugs whose glucose-lowering effect and cardiovascular and renal benefits were evidenced in clinical trials. We investigated the real-world efficacy and safety of the combination of SGLT2i and GLP-1RA in patients with type 2 diabetes mellitus in Korea. The medical records of 104 patients who maintained the combination for at least 1 year were retrospectively reviewed. The change in glycosylated hemoglobin (HbA1c) after 6 months and 1 year of treatment was evaluated. The mean age was 51 years, and 41% were female. The mean baseline HbA1c, body mass index, and duration of diabetes were 9.0%, 28.8 kg/m2, and 11.7 years, respectively. Compared with baseline, the HbA1c decreased by 1.5% (95% confidence interval [CI], 1.27 to 1.74; P<0.001) after 6 months and by 1.4% (95% CI, 1.19 to 1.70; P<0.001) after 1 year. Over 1 year, the bodyweight change was −2.8 kg (95% CI, −4.21 to −1.47; P<0.001). The combination of SGLT2i and GLP-1RA is effective and tolerable in type 2 diabetes mellitus patients in real-world practice.
-
Citations
Citations to this article as recorded by- Effectiveness and safety of the combination of sodium–glucose transport protein 2 inhibitors and glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of observational studies
Aftab Ahmad, Hani Sabbour
Cardiovascular Diabetology.2024;[Epub] CrossRef - Hormonal Gut–Brain Signaling for the Treatment of Obesity
Eun Roh, Kyung Mook Choi
International Journal of Molecular Sciences.2023; 24(4): 3384. CrossRef - All‐cause mortality and cardiovascular outcomes with sodium‐glucose Co‐transporter 2 inhibitors, glucagon‐like peptide‐1 receptor agonists and with combination therapy in people with type 2 diabetes
David R. Riley, Hani Essa, Philip Austin, Frank Preston, Isatu Kargbo, Gema Hernández Ibarburu, Ramandeep Ghuman, Daniel J. Cuthbertson, Gregory Y. H. Lip, Uazman Alam
Diabetes, Obesity and Metabolism.2023; 25(10): 2897. CrossRef - The Efficacy and Safety of the Combination Therapy With GLP-1 Receptor Agonists and SGLT-2 Inhibitors in Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis
Chen Li, Jie Luo, Mingyan Jiang, Keke Wang
Frontiers in Pharmacology.2022;[Epub] CrossRef - Clinical Efficacy of Sodium-Glucose Cotransporter 2 Inhibitor and Glucagon-Like Peptide-1 Receptor Agonist Combination Therapy in Type 2 Diabetes Mellitus: Real-World Study (Diabetes Metab J 2022;46: 658-62)
Hwi Seung Kim, Woo Je Lee
Diabetes & Metabolism Journal.2022; 46(4): 665. CrossRef - Clinical Efficacy of Sodium-Glucose Cotransporter 2 Inhibitor and Glucagon-Like Peptide-1 Receptor Agonist Combination Therapy in Type 2 Diabetes Mellitus: Real-World Study (Diabetes Metab J 2022;46: 658-62)
Tomoyuki Kawada
Diabetes & Metabolism Journal.2022; 46(4): 663. CrossRef - Durability of glucose-lowering effect of dulaglutide in patients with type 2 diabetes mellitus: A real-world data study
Hwi Seung Kim, Yun Kyung Cho, Myung Jin Kim, Chang Hee Jung, Joong-Yeol Park, Woo Je Lee
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Effectiveness and safety of the combination of sodium–glucose transport protein 2 inhibitors and glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of observational studies
- Drug/Regimen
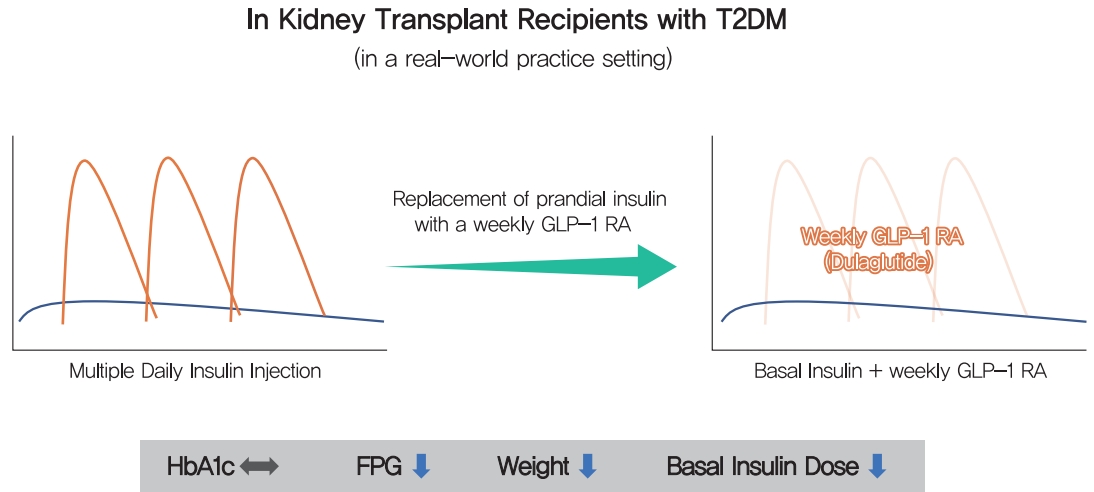
- Dulaglutide as an Effective Replacement for Prandial Insulin in Kidney Transplant Recipients with Type 2 Diabetes Mellitus: A Retrospective Review
- Hwi Seung Kim, Jiwoo Lee, Chang Hee Jung, Joong-Yeol Park, Woo Je Lee
- Diabetes Metab J. 2021;45(6):948-953. Published online February 5, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0180
- 5,787 View
- 232 Download
- 5 Web of Science
- 6 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Dulaglutide, a weekly injectable glucagon-like peptide-1 receptor agonist, has demonstrated effectiveness when combined with basal insulin. We examined whether the efficacy of dulaglutide is comparable to that of prandial insulin in kidney transplant (KT) recipients with type 2 diabetes mellitus (T2DM) undergoing multiple daily insulin injection (MDI) therapy. Thirty-seven patients, who switched from MDI therapy to basal insulin and dulaglutide, were retrospectively analyzed. Changes in glycosylated hemoglobin (HbA1c) and fasting plasma glucose (FPG) levels, body weight, and basal insulin dose were evaluated over 6 months. Dulaglutide was comparable to three injections of prandial insulin in terms of glycemic control (HbA1c 7.1% vs. 7.0%; 95% confidence interval [CI], –0.53 to 0.28; P=0.53). The basal insulin and dulaglutide combination resulted in a reduction in FPG levels by 9.7 mg/dL (95% CI, 2.09 to 41.54; P=0.03), in body weight by 4.9 kg (95% CI, 2.87 to 6.98; P<0.001), and in basal insulin dose by 9.52 IU (95% CI, 5.80 to 3.23; P<0.001). Once-weekly dulaglutide may be an effective alternative for thrice-daily prandial insulin in KT recipients with T2DM currently receiving MDI therapy.
-
Citations
Citations to this article as recorded by- Diabetic Kidney Disease in Post-Kidney Transplant Patients
Ngoc-Yen T. Pham, Diego Cruz, Luis Madera-Marin, Raja Ravender, Pablo Garcia
Journal of Clinical Medicine.2024; 13(3): 793. CrossRef - Safety and efficacy of glucagon-like peptide-1 receptor agonists among kidney transplant recipients: a systematic review and meta-analysis
Pajaree Krisanapan, Supawadee Suppadungsuk, Kanokporn Sanpawithayakul, Charat Thongprayoon, Pattharawin Pattharanitima, Supawit Tangpanithandee, Michael A Mao, Jing Miao, Wisit Cheungpasitporn
Clinical Kidney Journal.2024;[Epub] CrossRef - Sweet and simple as syrup: A review and guidance for use of novel antihyperglycemic agents for post‐transplant diabetes mellitus and type 2 diabetes mellitus after kidney transplantation
S. Elise Lawrence, Mary Moss Chandran, Jeong M. Park, Helen Sweiss, Thomas Jensen, Palak Choksi, Barrett Crowther
Clinical Transplantation.2023;[Epub] CrossRef - Novel Drugs for the Management of Diabetes Kidney Transplant Patients: A Literature Review
Nancy Daniela Valencia-Morales, Beatriz Rodríguez-Cubillo, Rómulo Katsu Loayza-López, Maria Ángeles Moreno de la Higuera, Ana Isabel Sánchez-Fructuoso
Life.2023; 13(6): 1265. CrossRef - Uso de los agonistas del receptor del péptido similar al glucagón tipo 1 en pacientes trasplantados renales
Luis Alberto Vigara, Florentino Villanego, Cristhian Orellana, Myriam Eady, María Gabriela Sánchez, Marta Alonso, María Belén García, José Manuel Amaro, Teresa García, Auxiliadora Mazuecos
Nefrología.2023;[Epub] CrossRef - Tolerability and Effectiveness of Switching to Dulaglutide in Patients With Type 2 Diabetes Inadequately Controlled With Insulin Therapy
Youngsook Kim, Ji Hye Huh, Minyoung Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Diabetic Kidney Disease in Post-Kidney Transplant Patients

 KDA
KDA
 First
First Prev
Prev





